Conditions
Abdominal Aortic Aneurysm
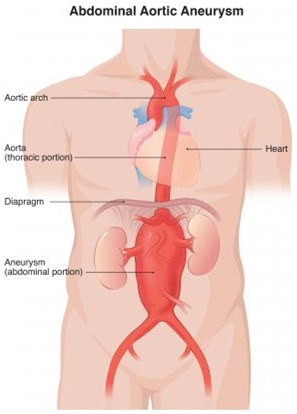
What is an aneurysm? An aneurysm occurs when the walls of your arteries weaken. The arteries form the pipework which carries blood around your body. The pressure of the flow of blood then makes the walls stretch and balloon out to form an “aneurysm”, which essentially means a weakened arterial wall segment which can burst.
Aneurysms can occur in any artery in the body. The most common location to have an aneurysm is in the aorta, which is the main artery in your tummy (abdomen). This is called an abdominal aortic aneurysm.
To get an idea of the location of the Aorta, imagining it running from your heart, down through the chest and into the tummy. At about the belly button area (or top of the hip level in overweight patients), it divides into 2 arteries (the iliac arteries) which deliver blood to the organs in your pelvis and your legs. These arteries can also form aneurysms, which often co-exist at the same time as abdominal aortic aneurysms.

Aneurysms do not just appear suddenly, but they grow larger with time (usually over several years). Therefore, smaller aneurysms can be fol- lowed-up with regular scanning and clinical examination in clinic, as they are not likely to rupture. However, depending on the location of the aneurysm, when it reaches a certain size the risk of it rupturing be- comes too great to just sit and watch. If an aortic aneurysm bursts this would result in massive internal bleeding, which is fatal for about 90 in every 100 people. At a certain width size of the aneurysm, your doctor may advise you to have it “repaired” surgically.
Ultrasound scan of the abdomen – able to measure the diameter of the aorta as shown above (black circle in the centre and below) The diagnosis is possible with clinical examination in thin patients and those with a size > 5 cm in diameter, so in the vast majority of cases it is confirmed with an ultrasound scan of the abdomen. The most important question that the scan addresses is the maximum diameter (external to external wall) of the aorta. The surgeon will also examine your groins and behind the knees to look for other aneurysms in the femoral and popliteal arteries.
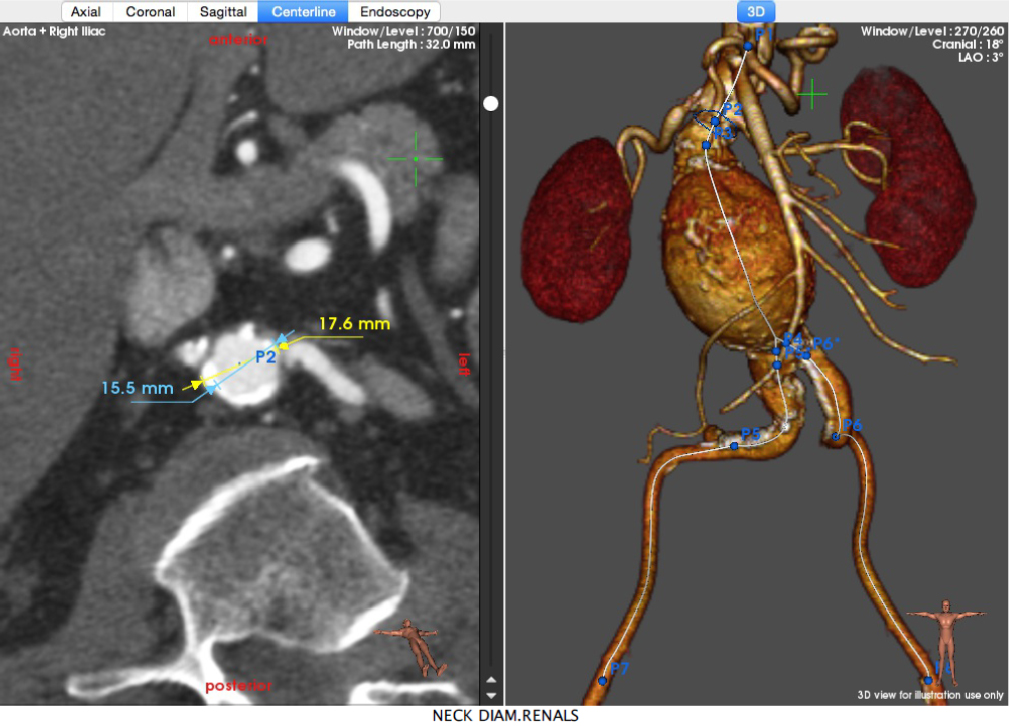
Once a surgeon needs more accurate information, either for diagnosis or for planning a repair, then a CT-Angiogram with intravenous contrast is requested as shown below:
Will I need an operation?
At some point an AAA may reach a size where surgery is indicated, usually when the aneurysm exceeds 5.5cm in men (and 5 cm in women). If the speed of growth is fast then a repair may be advisable even before the usual threshold of repair. Because surgery carries significant risks, the decision to operate must take into account the individuality of each patient’s health and reserves for recovery, in particular how well the heart, lungs and kidneys work. Before operating, most patients will need some sort of tests on these organs as well as routine blood tests to include FBC, ESR and electrolytes.
There is the minimally invasive endovascular aneurysm repair (EVAR) and the traditional open surgery. Data suggest that in patients with large AAAs (≥5.5 cm) undergoing elective repair, EVAR is equally “good” to open repair in terms of overall survival. In the short term, EVAR is less invasive and so it reduces AAA-related mortality and short-term complications and patients recover faster initially. The caveat is that with EVAR there must be life-long follow-up with scans (usually a scan 1 and 12 months after the repair, and then if all well every five years to detect leakage around the graft). The chance of needing further interventions (e.g. to repair the leakage) is higher than in Open repair. Decisions regarding repair should be individualised for each patient, taking account of patients’ preferences, patient age, quality of life, sex, the patient’s health reserves and anatomical / technical risk factors (not everybody is suitable for EVAR). Careful counselling must be undertaken regarding the risks of surgery and subsequent quality of life, with either of the two options. EVAR should be considered in patients who are unfit for traditional open surgery. Open traditional surgery for aneurysm repair is performed for between 10-30% of all AAA. It involves a vertical cut in the tummy and replacement of the diseased part of the aorta using an artificial tube called a graft. If the aneurysm extends into the iliac arteries, then a graft designed like a pair of trousers is used and may even have to extend to the groins in some, with separate cuts there. The main risk of surgery is death or heart attack, and this is about 1 in 20 patients overall. However, after a successful operation the risk of later complications is very low.
Many people never have problems from their AAA. But if an aneurysm does rupture, the chances of survival are small. That is why it is crucial to detect these aneurysms early, and to follow them up if they are small and not causing symptoms, or to have them repaired if a rupture seems more likely.
If you are having surgery, ask your doctor to give you the more detailed patient information leaflets for the type of surgery you will be undergoing.
The normal aorta is about 1.5 – 2.0 cm in width, the size of a garden hose
pipe. An abdominal aortic aneurysm is officially diagnosed if any part of
the aorta within the abdomen is 3 cm or more in diameter. If it is less than
that but greater than 2 cm then it is called Ectasia (not aneurysm) which is
not so concerning.
Aneurysms are often found by chance during a physical examination or a scan
for something else. They don’t often cause symptoms unless they have burst
or the blood inside them has clotted or sometimes, they press on a nearby
structure which gets affected and alerts the patient.
As they grow they may get so large that there is a significant chance of the
artery wall bursting and bleeding. This is a serious life-threatening
emergency known as a “ruptured aneu- rysm”.
Aneurysms can affect anybody, but they are more common in men, in people
suffering with high blood pressure (hypertension), in smokers and also in
people over the age of 65. Among UK men invited for screening at their 65th
birthday, about 1.5% of them have an abdominal aortic aneurysm (> 2.9 cm in
diameter). It is believed that about 1 to 3 in every 100 men over the age of
65 will develop an aneurysm, though not all will be of significant size, and
about 1 in 100 will have a large aneurysm requiring surgery. They are about
6 times rarer in women but once present, they are more likely to rupture in
women. The risk of developing an aneurysm appears to be in part hereditary
(that is, it depends on your genes). Close male relatives of an affected
patient are more likely to get one themselves. However, most patients do not
have a known family history and therefore genes are not wholly to be blamed
for this!
Smoking and high blood pressure are known to increase the size and risk, of
aneurysms once they are present.
AAA’s vary in size. As a rule, once somebody develops an AAA, it tends to
gradually get larger. The speed at which it gets larger varies from person
to person. It may be slowed down by taking certain medication (statins,
ACE-Inhibitors, Metformin, beta blockers) if suitable for you. Your doctor
will advise you. The risk of rupture at each diameter can be summarized
broadly in the Table below:
| Size of aorta | Description | Risk of rupture/ year |
|---|---|---|
| 4cm or less | not an aneurysm | no real risk |
| 4 - 5cm | small aneurysm | about 1 in 100 |
| 5 - 6cm | AAA | about 1 in 12 |
| 6 - 7cm | large aneurysm | about 1 in 6 |
| over 7cm | very large aneurysm | about 1 in 4 or higher |
 EVAR is “keyhole” type of surgery where the aneurysm in your tummy is repaired using a special stent. A fabric covered stent with wire support is fitted inside the aorta to strengthen it, preventing blood from flowing through the aneurysm, which gradually should shrink if blood does not flow through it. It can be done under general or even regional anaesthesia with the patient awake and it involves accessing the aorta through the groin area, with small cuts. The risk of death following EVAR is about 2 in every 100 which is lower than traditional open surgery discussed above. Around 10 in 100 patients will need to have a further smaller operation in the future if a leak is detected around the stent at follow-up. General complications of this type of surgery include a heart attack and chest infection, but these are rare.
EVAR is “keyhole” type of surgery where the aneurysm in your tummy is repaired using a special stent. A fabric covered stent with wire support is fitted inside the aorta to strengthen it, preventing blood from flowing through the aneurysm, which gradually should shrink if blood does not flow through it. It can be done under general or even regional anaesthesia with the patient awake and it involves accessing the aorta through the groin area, with small cuts. The risk of death following EVAR is about 2 in every 100 which is lower than traditional open surgery discussed above. Around 10 in 100 patients will need to have a further smaller operation in the future if a leak is detected around the stent at follow-up. General complications of this type of surgery include a heart attack and chest infection, but these are rare.