Conditions
EVLA
EVLA is one of the modern, but well tested and tried, evidence-based methods of treating varicose veins without surgery. Alternative options for treating varicose veins include: no treatment, compression stockings, surgery or injections into the varicose veins (sclerotherapy). Other methods such as using microwave energy to destroy the vein instead of laser and sealing the veins with glue are also available.
EVLA has come into widespread use in specialist centres since 2004 and it has been perfected in the last 15 years. It is a quick, minimally invasive alternative to traditional vein stripping. A laser fibre is inserted into the vein and the vein is destroyed by laser energy heating the inside of the vein (typically 8W, which is much less than the power of a lightbulb). The procedure is performed through a tiny cut at the knee level, usually only 1-2mm long. The procedure is performed with local anaesthetic. Several local anaesthetic injections in the leg are necessary. These are uncomfortable, but the discomfort does not last for long. The body then naturally absorbs the destroyed veins. It avoids scarring and bleeding and can be performed under local anaesthesia and light sedation if the patient wants to avoid a general anaesthetic. It has a much shorter recovery time than surgery and patients can walk out within a couple of hours. Some patients request to also have the smaller bulging veins in the leg removed through tiny cuts (avulsions). These cuts are usually closed with adhesive tape. These are performed after the laser part of your treatment has taken place. Not all patients require this part of the operation but you can discuss this with your surgeon.
Need content for this section
Ultrasound scanning before the procedure may reveal that your varicose veins are not suitable for EVLA. Most often this is because the vein is twisting a lot along its length (zig-zag or small recurrent veins after previous surgery) or multiple little hardened clots are found inside (superficial thrombophlebitis due to inflammation of the vein). Most patients (8 out of 10) with troublesome varicose veins are suitable for EVLA. Those who are not suitable can usually be managed with ultrasound guided foam sclerotherapy. EVLA is not recom- mended for people who are unable to walk; in poor general health; have a clotting disorder or are pregnant.
Patients can walk immediately after the procedure and may be allowed home within a few hours after the end of treatment. You may have to wear compression stockings (and / or bandages for the first 4 days) for up to 2 weeks. You should resume normal activity as soon as possible, normally within 2-3 days. Hot baths and vigorous activity such as gym workouts should be avoided in the first 2 weeks. Pain and discomfort for most patients are minimal and usually improve within a few days but can last for longer in others. Flying and excessively long journeys should be avoided for the first 4 weeks due to a slightly increased risk of deep vein thrombosis (DVT). Most patients experience some bruising or pain for up to 2 weeks, or a tightening sensation along the length of the treated vein but this is usually mild. Simple painkillers like paracetamol and anti-inflammatory drugs like Ibu- profen relieve it very well.
If patients are having treatment just to relieve symptoms then no further treatment beyond the laser of the main vein is usually necessary. Most patients however wish also to improve the appearance of their veins and of these about 80% will require further treatment to achieve that. The main varicosities normally become much less obvious after EVLA but all varicosities rarely disappear completely. Additional treatment for these smaller varicosities can be either by avulsions (phlebectomies) under local anaesthetic or foam sclerotherapy in the outpatient clinic. These additional treatments can be undertaken more usually after a delay of 6 weeks, because this is the time it takes for the effect of EVLA to show. Foam sclerotherapy is the commonest means of dealing with residual varicose veins after EVLA and is highly effective for these.
There are potential complications with any medical procedure. Minimal
complications have been experienced with the endovenous laser procedure as
it is minimally invasive. Serious complications after EVLA are very rare.
Sometimes the procedure cannot be completed as planned and has to be
postponed for a later date. This can happen in less than 1 in 100 cases with
both EVLA and foam sclerotherapy when it becomes technically impossible to
get access to the veins or to position the instruments correctly through the
vein.
With EVLA expect to have a significant amount of bruising along the thigh.
Wearing compression stockings (or bandages) for 4 days and nights initially
and then compression stockings for another 10 days (during the day only)
helps significantly to minimise the bruising and any discomfort. Another
common side effect occurring in most patients is a feeling of tightness
along the length of the vein on the inner aspect of the thigh as the vein
contracts over the first 4 weeks. In some patients this can be uncomfortable
enough to warrant taking some simple anti-inflammatory tablets, like
Ibuprofen (e.g. nurofen) which will usually relieve it adequately.
Occasionally you can develop some thread veins following EVLA, normally
along the course of the vein that has been lasered but can be in other
locations on the leg. If this occurs, then you will require
microsclerotherapy injections to clear these up in the outpatients clinic.
This is a separate cosmetic procedure.
More serious complications are very rare with EVLA but in theory, it would
be possible for any of the following to occur:
1. Deep Vein thrombosis and pulmonary embolism. This is the development of a
clot occurring in the large deep veins inside the leg or lower tummy. If
such a clot travels up to the lungs, this is called a pulmonary embolism,
which can cause pain in the chest, breathlessness and even death. We advise
all our patients to walk at least 45-60 minutes everyday for the first week
after the procedure which from experience seems to afford them excellent
protection.
2. Skin burns. This was reported in the scientific literature in the first
cases of using the laser machinery 15 years ago
3. Nerve damage. It is not surprising that nerves lying close to the veins
having treatment may be damaged, leading to patches of numbness or tingling
on the skin, but it is usually mild and temporary. Very rarely does this
persist for longer than 3 months.
4. Leg swelling
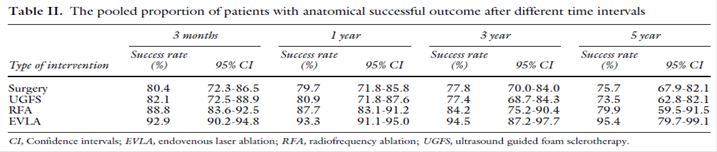
EVLA / Foam sclerotherapy may not be suitable for all patients (but up to 90% of them) and there will be some in whom other treatments (including doing nothing, wearing surgical stockings, using cosmetics, open surgery or Clarivein) are more appropriate. Stockings (knee and thigh-length) are effective in controlling symptoms and preventing skin compli- cations. They are only effective if worn regularly but can reliably avoid the need for surgery in some patients. The newer minimally invasive methods appear to have broadly similar results with open surgery and a recent comparison of relevant published studies has shown the variability of the results for each type of treatment (shown below, Table II taken from a metanalysis by Van Den Bos R et al, J Vasc Surg 2009; 49: 230-239).
THE 5 YEAR RESULTS OF EVLA WITH AN AVERAGE 95% SUCCESS RATE ARE VERY PROMISING:
There are several options including doing nothing, having an open operation and several new non-surgical treatments like Foam Sclerotherapy, radiofrequency ablation (RFA), superglue and EVLA. Much will depend on the experience and recommendation of your vascular specialist. Doing nothing is a good option if you are not bothered by the appear- ance of your veins and they are not causing significant symptoms. There is no medical need to treat most varicose veins. Wearing stockings is a good option for those with symp- toms but who are not worried about the appearance of their legs and are willing to wear stockings for the rest of their lives. Open surgery has been performed for decades and it is still preferred by some patients. If a patient wants to avoid open surgery and general anaesthesia and to get back to normal activities quickly they should consider one of the minimally invasive treatments. Discuss together with your vascular surgeon before coming to a decision about which treatment is right for you. No single treatment is the best for every- body. In fact, quite a few patients may need a combination of 2-3 treatment methods to achieve the best results for their individual needs.
Simple measures such as wearing appropriate compression stockings will control the symptoms for many people. Stockings may help to prevent progression or enlargement of vari- cose veins. If you are overweight you should try to lose weight. Regular exercise is the best gift of health you can give to your legs!